Headache and Migraines: Everything You Should Know

Written by Dr. Ruby Rose, MD.
In this month’s pain series I’d like to address one of the most common pain complaints, headache. Primary Headache Disorders don’t have one underlying cause and include migraine, tension-type headaches and cluster headaches while Secondary Headache Disorders have an underlying cause and are what many physicians try to rule out as possible causes such as brain tumors or hemorrhages. For the purposes of this edition, I plan to focus on primary headaches.
Primary Headache Types
1. Tension-Type Headache
Tension-Type Headache is the most common headache disorder and are described as mild to moderate bilateral tightening of one’s head and does not typically cause nausea/vomiting or worsen with activity.
2. Migraine Headaches
Migraine Headaches typically last hours to days and are described as unilateral, throbbing/pulsating, moderate to severe in intensity; are worse with activity, and can include nausea/vomiting and photo/phonophobia (light and sound sensitivity). Some will describe visual or sensory symptoms prior to pain (auras). Women are 3 times more likely to suffer from chronic migraines.
3. Cluster Headaches
Cluster Headaches are more rare and are described as severe rapid onset of pain typically around or behind the eye causing tearing or eye redness, eyelid drooping, nasal congestion, sweating and restlessness, and lasts 1-3 hours. These are more common in men.
4. Medication Overuse Headache
One other type of headache worth mentioning is Medication Overuse Headache, which is a rebound headache that can be daily and caused by one or more drugs overused regularly for over 3 months.
The most common drugs include butalbital, opioids, Tylenol, caffeine and NSAIDs (most commonly in the form of combination medications). Once these meds are carefully weaned, the headaches resolve.
See also: Houston ER Doctor Advises Heat safety as Texas Summer Temperatures Set to Soar.
Conventionally, headaches are treated with over the counter abortive medications such as NSAIDs or Tylenol, or with prescriptions such as triptans, anti-nausea medications and narcotics. Preventive medications can include the abortive options mentioned above plus cardiac, anti-seizure and antidepressant meds and botox. Tension-type headaches don’t typically require prescription medication due to their infrequency.
Due to the varying side effects of many of these medications, it is no wonder that over 80% of patients seek alternative therapies. Integrative approaches such as lifestyle, mind-body, herbs and supplements along with manual therapies have produced the most evidence for the effective treatment of primary headache disorders.
What Is Causing My Headache
The mechanism by which a migraine develops and persists still remains a mystery and is thought to be driven by environment, lifestyle and genetic factors. We do know that the pathophysiology of migraines involves the connection between the vascular, trigeminal and neuroendocrine systems and has a strong genetic (i.e. methylation dysfunction) and epigenetic influence (nutrient deficiencies and toxins).
Tension-type headaches are thought to be caused by sensitization of the peripheral nerves of the skull and upper neck.
Identifying Headache Triggers
It is theorized that several triggers are involved in crossing the migraine threshold leading to pain, further suggesting that there is not just one underlying cause for primary headaches.
As we learn more about the role of our gut microbiome, more research is revealing the gut-brain axis as a modulator of pain. Patients with inflammatory bowel disease (IBD) are twice as likely to have migraines in addition to those with IBS, gastroparesis and liver/gallbladder diseases.
Identifying the trigger can sometimes be the single most effective treatment, particularly in children. The most common trigger for migraine is emotional stress followed by poor sleep quality.
Environmental Triggers
Environmental triggers can include air toxins (perfumes, sprays, smoke), cold weather, humidity, bright lights.
Dietary Triggers
Dietary triggers include processed foods with nitrates and nitrites (see link below), dyes, MSG, aspartame; food allergies (i.e. gluten), alcohol, caffeine; fasting and dehydration.
Other Triggers
Other triggers include varying hormone levels, particularly estrogen, during menarche, menstrual cycles, perimenopause or hormone replacement.
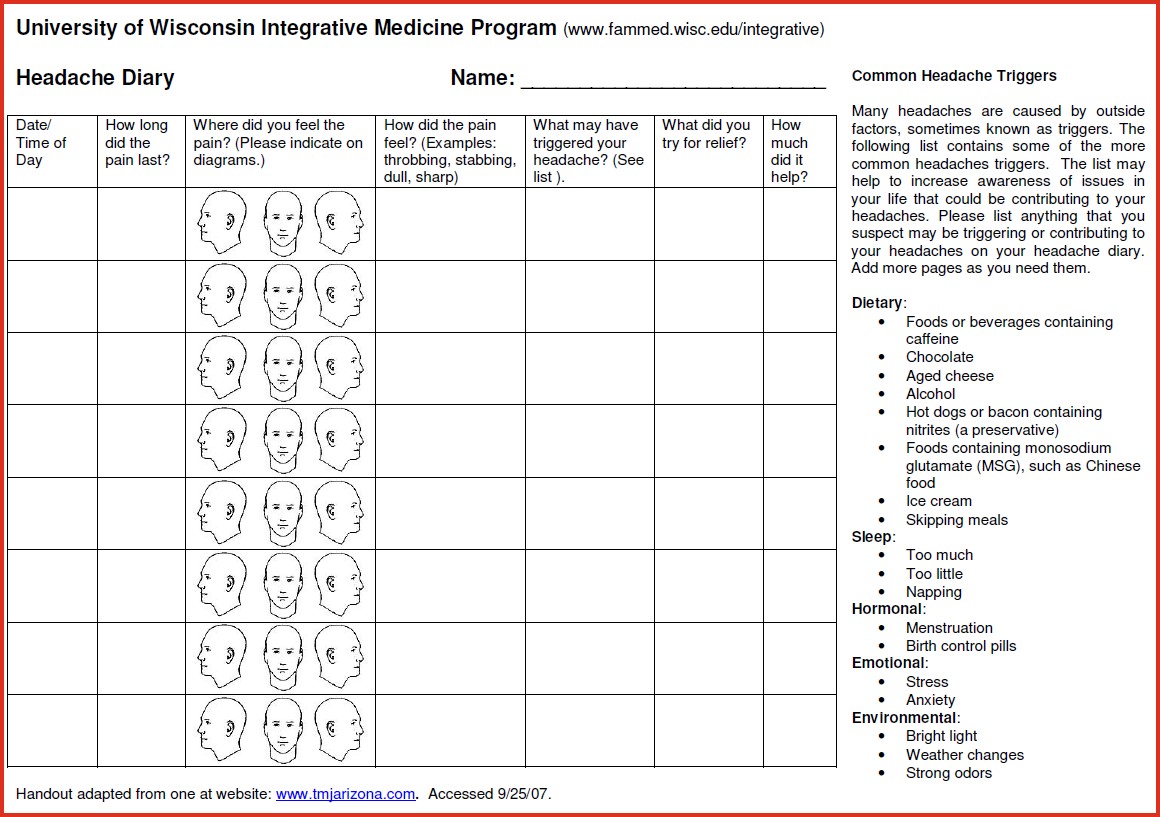
I suggest starting a headache diary to help zone in potential triggers (see below).
Integrative Medicine Approaches to Headache
Mind-Body Approaches
- Acupuncture was found to have a significant impact on the frequency of tension headache and migraine attacks.
- Visualization Breath Work taps into the parasympathetic system (relaxation) and promotes stress reduction, oxygenation and pH balancing.
- PEMF (pulsed electromagnetic field) therapy has been shown to positively and non-invasively treat migraines at the cellular and mitochondrial level.
- Craniosacral Therapy, spinal manipulation, massage and TMJ therapy has been effective for treatment of both migraines and tension-type headaches. Teeth grinding can exacerbate both migraine and tension headache, so introducing a mouth guard can make a tremendous impact.
Supplements
Deficiencies in the below compounds are frequently noted in those with migraines. In addition, there is growing evidence that mitochondrial dysfunction is one of the mechanisms by which migraines develop. Many of the recommended supplements below support mitochondrial health and energy. All of the supplements can also be obtained from fresh whole food sources.
Remember, you can’t supplement out of a bad diet and sedentary lifestyle!
- Magnesium100-600mg/day with food: strong research and support for use in migraine and menstrual migraines. Mg glycinate and malate are probably the gentlest on the gut and help with general pain reduction.
- Activated B-Vitamins and Vitamin D3
- CoQ10 300 mg/d: reduces inflammation and oxidative stress. (Best if taken in the form of liposomal ubiquinol).
- Additional supplements that have shown to help prevent and reduce frequency of attacks include L-carnitine, alpha lipoid acid (ALA) and melatonin.
Botanical Approaches
- Petadolex® (Butterbur extract) is generally well tolerated and safe for migraine treatment.
- Feverfew is an herb shown to be safe and effective for chronic headache but longterm use and abrupt cessation can cause rebound headache. The combination of feverfew and ginger particularly in the sublingual form was found to be even more beneficial.
- Ginkgo biloba leaf (120-240 mg/d) is an antioxidant and anti-inflammatory option for reducing frequency of migraines and aura symptoms.
* With any of my recommendations, if you are pregnant or have any chronic condition (i.e. liver or kidney disease), please consult with your provider. *
Summary
- Identify your trigger.
- Try not to go cold turkey on caffeine or other medications if you decide you’d like to stop a medication.
- Consider food allergies and try an elimination diet. As foods are added back in after 3-4 weeks, pay attention to what triggers a headache.
- Start supplementing with activated b-vitamins, vitamin D3 and methylated folate. Check to see if you are anemic.
- Diets high in omega 3 fatty acids (such as the Mediterranean and Anti-Inflammatory diet) are the most beneficial for reducing pain and headaches.
- Leaky gut can lead to leaky brain so addressing your gut health is crucial.
- Seek activities that promote stress reduction and sleep quality.
- Remove toxins: use air and water filters; limit metals from fish (older deep sea fish like tuna and swordfish).
Suggested Reading
- One of my favorite books recently is Genius Life by Max Lugavere. He made 2 delicious cookbooks I highly recommend as a staple in your kitchen: Genius Foods and Genius Kitchen.
- If you’re looking for a bedside book of reflections, the quote above is from this book: Consolations. The Solace, Nourishment and Underlying Meaning of Everyday Words by David Whyte.
Other Articles by Dr. Ruby Rose, MD -
GERD (Heartburn) – Pain in the Upper Gut
Maximizing Wellness During a Pandemic
-----------------------------------------------------------------
 Dr. Ruby Rose, MD, is board certified in emergency medicine. She is currently the Medical Director of SignatureCare Emergency Center, Austin, TX. Originally from New York City, Dr. Rose graduated from Vassar College in New York before obtaining her medical degree from Tufts University School of Medicine in Boston, Massachusetts. She completed her emergency medicine residency at University of Massachusetts. Dr. Rose has a passion for alternative care and recently graduated from the University of Arizona Integrative Medicine Fellowship in Tucson, Arizona. After relocating to Texas with her family, Dr. Rose worked in St. David’s Healthcare System where she served in several leadership positions. In her spare time, she enjoys watching her kids play various sports and riding her horse in the Texas Hill Country.
Dr. Ruby Rose, MD, is board certified in emergency medicine. She is currently the Medical Director of SignatureCare Emergency Center, Austin, TX. Originally from New York City, Dr. Rose graduated from Vassar College in New York before obtaining her medical degree from Tufts University School of Medicine in Boston, Massachusetts. She completed her emergency medicine residency at University of Massachusetts. Dr. Rose has a passion for alternative care and recently graduated from the University of Arizona Integrative Medicine Fellowship in Tucson, Arizona. After relocating to Texas with her family, Dr. Rose worked in St. David’s Healthcare System where she served in several leadership positions. In her spare time, she enjoys watching her kids play various sports and riding her horse in the Texas Hill Country.




