By Dr. Christopher L Huerta, MD
Imagine a tiny, unseen predator, barely a whisper in the twilight breeze. It lands silently, delivers a microscopic injection, and then, just as quickly, is gone.
You might not feel a thing, or perhaps a slight itch, easily dismissed. But that seemingly insignificant encounter could be the start of a fight for your very neurological future. This is the insidious reality of the West Nile Virus (WNV) in Texas, a silent threat that can leave a devastating mark on your life, your family, and your community.
As of July 2025, West Nile virus is not a theoretical threat; it is an active presence across Texas, with confirmed human cases and infected mosquitoes signaling a season of vigilance and potential danger. The first human case of the season was identified in Brazos County on June 24, 2025, a stark reminder that this viral menace is here, now, and ready to strike. The virus has since spread, with confirmed cases reported in 14 Texas counties, from Brazos to Williamson, touching communities across the state.
-----------------------------------------------------------------------------
What You Should Know About West Nile Virus in Texas
- First human case of West Nile Virus in 2025 has been reported in Texas
- By July 2025, 14 Texas counties including Brazos, Collin, Dallas, Denton, Fort Bend, Harris, Johnson, Lubbock, Montgomery, Randall, Tarrant, Travis, Wichita, and Williamson have confirmed positive cases
- The mosquito season, and therefore West Nile Virus activity, typically increases during warmer months, peaking from May through October, and can extend into November and December in much of Texas.
- In 2024, Texas reported 455 cases of West Nile disease and 56 deaths
- Over the past five years (2020-2024), there have been 929 cases and 122 deaths reported in the state, according to the Texas Department of State Health Services (DSHS).
- 2,274 WNV cases were reported in Texas between 2002 and 2011. The most significant outbreak to date occurred in 2012, when 1,868 cases were reported. This number was more than double the previous high of 735 cases in 2003.
- While WNV has been found in 53% of Texas counties, nearly half of all cases reported in 2012 came from the Dallas/Fort Worth metropolitan area.
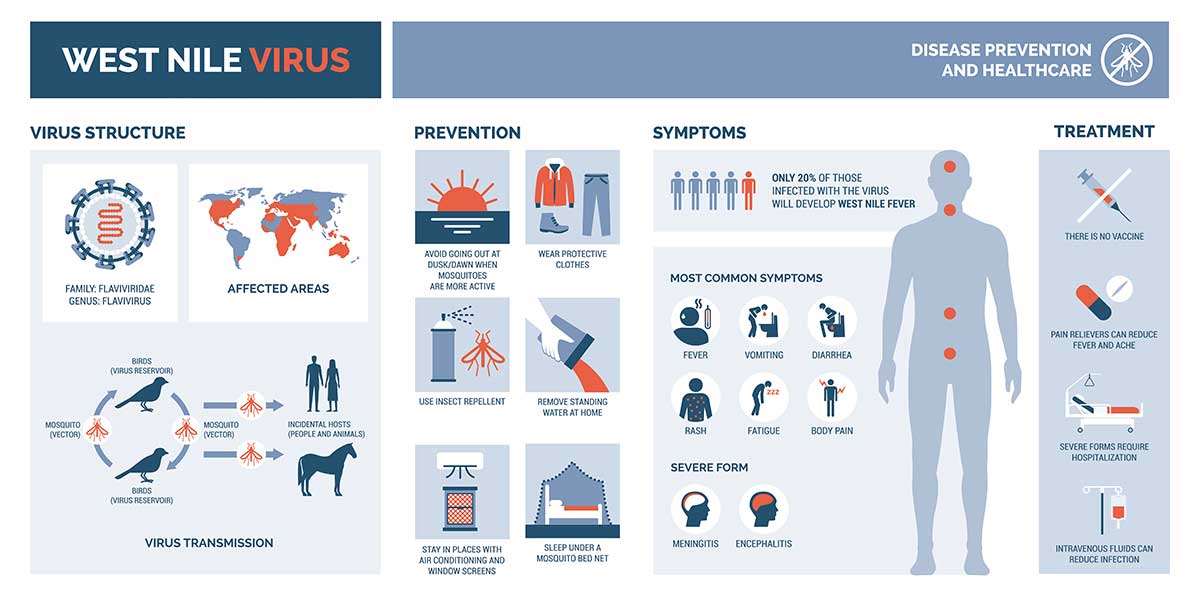
- Most people (about 80%) infected with WNV will not experience any symptoms
- Roughly 20% of infected individuals may experience symptoms of West Nile Fever, which can include fever, nausea, headache, fatigue, and muscle and joint pain
- A small percentage (less than 1%) may develop more severe symptoms affecting the nervous system, potentially leading to disorientation, neck stiffness, tremors, paralysis, convulsions, or even death.
- Only you can prevent yourself and family from contracting West Nile Virus.
-----------------------------------------------------------------------------
The Texas Department of State Health Services (DSHS) paints a sobering picture: in 2024 alone, there were 455 reported cases of West Nile disease and 56 deaths. Over the last five years, from 2020 to 2024, the toll has reached 929 cases and a heartbreaking 122 deaths.
These numbers represent individuals whose lives, and the lives of their loved ones, have been irrevocably altered. A mosquito bite, barely noticed, can trigger a cascade of events leading to severe illness, lifelong disability, or even death. This is why understanding West Nile Virus, recognizing its symptoms, and knowing when to seek immediate emergency care is not merely recommended, it is a matter of life and death.
Understanding West Nile Virus, the Unseen Enemy
Origins and Arrival in the Lone Star State
The story of West Nile virus begins far from the Texas prairies, tracing back to the West Nile District of Uganda in 1937. It traveled across continents, through Africa, the Middle East, Europe, and Asia, a quiet menace on the global stage. Its arrival in the United States in 1999, during an outbreak of encephalitis in New York, marked a new chapter in the virus's journey, setting the stage for its eventual spread across the entire continent, including Central and South America, and parts of Canada.
Texas recorded its first human cases in 2002. Since then, WNV has become endemic in Texas, meaning it is consistently present within the local bird and mosquito populations. Mosquito season, typically peaking from May through October, sees a surge in WNV activity, sometimes extending into the milder months of November and December in many parts of the state.
How West Nile Virus Spreads
The West Nile virus is primarily transmitted to humans through the bite of an infected mosquito. The virus lives within a cycle involving birds and mosquitoes, particularly those from the Culex genus, a type of mosquito abundant in Texas.
These mosquitoes become infected when they feed on the blood of birds carrying the virus. If a mosquito then bites a human, horse, or other animal, it can transmit the virus, effectively acting as a bridge between the infected bird population and susceptible hosts. It's crucial to remember that West Nile Virus cannot be spread from person to person, except in very rare cases, such as during pregnancy, breastfeeding, blood transfusion or organ transplant.
Recognizing the Symptoms of West Nile Virus
The true danger of West Nile virus lies in its stealthy nature. Most people who are infected will not experience any symptoms at all, a quiet incubation that can breed complacency. However, a significant minority will fall ill, and for some, the consequences can be catastrophic.
The Flu-Like Falsehood: West Nile Fever
Approximately 20-25% of individuals infected with West Nile Virus will develop a milder illness known as West Nile fever. This stage can be deceptive, mimicking common ailments like the flu, with symptoms that can include:
- Fever
- Headache
- Body aches and muscle pain
- Joint pain
- Fatigue and general weakness
- Nausea and vomiting
- Diarrhea
- Skin rash (often appearing as small, flat or raised, pink to red spots on the trunk, potentially spreading to arms and legs)
- Swollen lymph glands
- Sore throat
- Pain behind the eyes
While most people recover completely from West Nile fever, some may experience lingering fatigue and weakness for weeks or even months. This initial phase can be easily dismissed, but it's a critical juncture. It's like seeing the warning lights on your car's dashboard – ignore them at your peril.
West Nile Neuroinvasive Disease (WNND)
West Nile Neuroinvasive Disease (WNND), the most severe form of the illness, develops in less than 1% of individuals infected with West Nile virus. This occurs when the virus penetrates the body's defenses and attacks the central nervous system.
This leads to potentially life-threatening inflammation of the brain (encephalitis), the membranes surrounding the brain and spinal cord (meningitis), or even the spinal cord itself, mimicking poliomyelitis.
Symptoms of West Nile Neuroinvasive Disease (WNND)
The symptoms of West Nile Virus are severe and require immediate action. Do not hesitate if someone you know experiences any of the following symptoms or illnesses. Call 911 or seek emergency medical care immediately.
Excruciating Headache: Unlike a typical headache, this is an unrelenting pain, a warning sign of a potential crisis.
High Fever: A temperature above 101°F (38.3°C) is a serious indicator.
Stiff Neck: Difficulty touching the chin to the chest can be a sign of meningeal irritation.
Confusion or Disorientation: The mind becomes foggy, with difficulty recognizing familiar faces or places, losing track of time, or struggling to maintain a coherent conversation.
Seizures or Tremors: Uncontrollable shaking or muscle movements are a sign that the virus is impacting brain function.
Loss of Movement or Paralysis: Weakness in a limb, partial paralysis, or complete loss of movement, especially when there are no other obvious causes, is a critical emergency. Infections of the spinal cord can cause poliomyelitis-like symptoms, with damage to anterior horn cells and a potential for respiratory paralysis requiring mechanical ventilation.
Vision Changes: Blurred vision, sensitivity to light, or other sudden visual disturbances can indicate neurological complications.
Unusual Sleepiness or Difficulty Waking Up: A change in consciousness, from stupor to coma, is a sign of a severe neurological event.
Do not delay seeking medical attention if these symptoms arise. Rapid diagnosis and supportive care can make a difference between recovery and lifelong neurological impairment, or even death.
Long-Term Consequences of West Nile Disease
Even for those who survive West Nile Neuroinvasive Disease, the battle might not be over. Research, including a 10-year study of West Nile Virus patients, has revealed that long-term neurological complications are a significant concern, with nearly half of patients experiencing some form of abnormality. These include:
Motor Dysfunction: Muscle weakness, tremors, and balance and coordination problems are common long-term effects. Some individuals may need assistive devices.
Memory Loss and Cognitive Impairment: Difficulty with short-term and long-term memory, attention deficits, and executive dysfunction have been reported. Brain scans have even revealed physical changes, such as shrinkage or thinning in areas of the cerebral cortex responsible for these higher-level abilities.
Depression and Anxiety: Depression can develop in a significant percentage of survivors. The incidence of major depressive disorder among survivors ranges from 21% to 56%.
Fatigue and Malaise: Persistent, debilitating fatigue can plague survivors for months or even years, impacting their ability to resume normal activities.
Hearing Loss: Some individuals may experience decreased hearing or other auditory issues.
The consequences of a simple mosquito bite can be devastating, potentially altering who you are.
Consider the story of David Lemoine, a Texas attorney. West Nile virus changed his voice and body, leaving him with a frozen vocal cord, paralysis, and an inability to lift more than 25 pounds.

Treatment and Prevention of West Nile Disease
There is no specific cure for West Nile virus, and no vaccine is currently available for humans.
Treatment focuses on supportive care, helping the body fight the infection and manage symptoms. This often involves hospitalization for severe cases, where patients may receive intravenous fluids, pain medication, and careful monitoring of vital signs and neurological function.
In some cases, treatments like intravenous gamma globulin, containing antibodies from West Nile Virus survivors, have shown promise in small trials.
However, the best defense is prevention. Individuals can protect themselves and their families from this unseen threat by taking simple, proactive measures.
West Nile Virus Preventive Measures
You can take several steps to protect yourself and family from West Nile Virus.
Drain Standing Water: Mosquitoes breed in stagnant water. Regularly remove water from flowerpots, gutters, birdbaths, old tires, and any other containers where water can collect. Change the water in pet dishes daily and in wading pools and bird baths several times a week.
Use EPA-Approved Insect Repellent: Apply repellents containing DEET, picaridin, IR3535, oil of lemon eucalyptus, or para-menthane-diol when outdoors, especially during peak mosquito activity (dawn and dusk). Always follow the product label instructions carefully.
Dress Defensively: Wear long sleeves and pants, especially during dawn and dusk, to create a physical barrier against mosquito bites.
Keep Mosquitoes Out: Ensure window and door screens are in good repair or keep them closed. Air conditioning can also help keep mosquitoes out of your home.
Be Aware: Stay informed about West Nile Virus activity in your area. Local health departments often provide updates on mosquito surveillance and human case counts.

When to Seek Emergency Care for West Nile Virus
The risk of developing severe, life-altering complications is real and ever-present during mosquito season. The danger is particularly elevated for individuals over 50 years old and those with compromised immune systems or underlying chronic conditions like diabetes or hypertension (high blood pressure).
The story of Rebecca Bollman, a young Texas A&M student whose life was derailed by West Nile encephalitis, is a reminder of this. She woke up in the hospital, learning to walk, talk, and function all over again. Scott Sechelski, a healthy father of two, needed a walker and struggled with shaky hands after his battle with West Nile. These are reminders of the destructive potential of this disease.
If someone develops symptoms that could indicate West Nile virus, particularly the severe neuroinvasive symptoms mentioned above (severe headache, high fever, stiff neck, confusion, seizures, loss of movement, vision problems), do not hesitate.
Call 911 or go to the nearest emergency room immediately.
Early diagnosis and prompt supportive care can significantly impact the outcome, potentially mitigating long-term damage and improving the chances of recovery.
The typical emergency room is equipped to handle these serious situations, providing the necessary tests (blood tests, spinal fluid analysis, imaging scans) and supportive treatment to help combat the virus.
Final Thoughts
West Nile virus is a dangerous foe in Texas, and it's up to everyone to be vigilant and proactive. By understanding the risks, recognizing the symptoms, and taking decisive action, when necessary, we can protect ourselves, our families, and the community from the potentially devastating consequences of West Nile virus. Don't let a mosquito bite become a tragic turning point. Stay informed, stay protected, and seek emergency medical care without delay if in doubt. The health and potentially the life of anyone affected could depend on it.
-----------------------------------------------------------------------------
Dr. Christopher L Huerta, MD, is a board-certified emergency medicine specialist based in Midland, TX, and the Medical Director of SignatureCare Emergency Center in Midland, TX. He received his medical degree from Washington University in St. Louis School of Medicine and has been in practice for more than 40 years.










